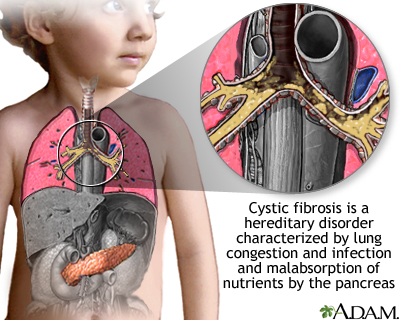
Cystic fibrosis is a disease that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body. It is one of the most common chronic lung diseases in children and young adults. It is a life-threatening disorder.
Causes
Cystic fibrosis (CF) is a disease that is passed down through families. It is caused by a defective gene that makes the body produce abnormally thick and sticky fluid, called mucus. This mucus builds up in the breathing passages of the lungs and in the pancreas.
The buildup of mucus results in life-threatening lung infections and serious digestion problems. The disease may also affect the sweat glands and a man's reproductive system.
Many people carry a CF gene, but do not have symptoms. This is because a person with CF must inherit 2 defective genes, 1 from each parent. Some Americans have the CF gene. It is more common among those of northern or central European descent.
Most children with CF are diagnosed by age 2, especially as newborn screening is performed across the United States. For a small number, the disease is not detected until age 18 or older. These children often have a milder form of the disease.
Symptoms
Symptoms in newborns may include:
- Delayed growth
- Failure to gain weight normally during childhood
- No bowel movements in first 24 to 48 hours of life
- Salty-tasting skin
Symptoms related to bowel function may include:
- Belly pain from severe constipation
- Increased gas, bloating, or a belly that appears swollen (distended)
- Nausea and loss of appetite
- Stools that are pale or clay-colored, foul smelling, have mucus, or that float
- Weight loss
Symptoms related to the lungs and sinuses may include:
- Coughing or increased mucus in the sinuses or lungs
- Fatigue
- Nasal congestion caused by nasal polyps
- Repeated episodes of pneumonia (symptoms of pneumonia in someone with cystic fibrosis include fever, increased coughing and shortness of breath, increased mucus, and loss of appetite)
- Sinus pain or pressure caused by infection or polyps
Symptoms that may be noticed later in life:
- Infertility (in men)
- Repeated inflammation of the pancreas (pancreatitis)
- Respiratory symptoms
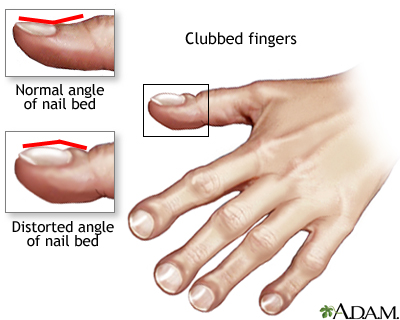
- Clubbed fingers
Exams and Tests
A blood test is done to help detect CF. The test looks for changes in the CF gene. Other tests used to diagnose CF include:
- Immunoreactive trypsinogen (IRT) test is a standard newborn screening test for CF. A high level of IRT suggests possible CF and requires further testing.
- Sweat chloride test is the standard diagnostic test for CF. A high salt level in the person's sweat is a sign of the disease.
Other tests that identify problems that can be related to CF include:
- Chest x-ray or CT scan
- Fecal fat test
- Lung function tests
- Measurement of pancreatic function (stool pancreatic elastase)
- Secretin stimulation test
- Trypsin and chymotrypsin in stool
- Upper GI and small bowel series
- Lung cultures (obtained by sputum, bronchoscopy or throat swab)
Treatment
An early diagnosis of CF and treatment plan can improve both survival and quality of life. Follow-up and monitoring are very important. When possible, care should be received at a cystic fibrosis specialty clinic. When children reach adulthood, they should transfer to a cystic fibrosis specialty center for adults.
Treatment for lung problems includes:
- Antibiotics to prevent and treat lung and sinus infections. They may be taken by mouth, or given in the veins or by breathing treatments. People with CF may take antibiotics only when needed, or all the time. Doses are often higher than normal.
- Inhaled medicines to help open the airways.
- Other medicines that are given by a breathing treatment to thin mucus and make it easier to cough up are DNAse enzyme therapy and highly concentrated salt solutions (hypertonic saline).
- Flu vaccine and pneumococcal polysaccharide vaccine (PPV) yearly (ask your health care provider).
- Lung transplant is an option in some cases.
- Oxygen therapy may be needed as lung disease gets worse.
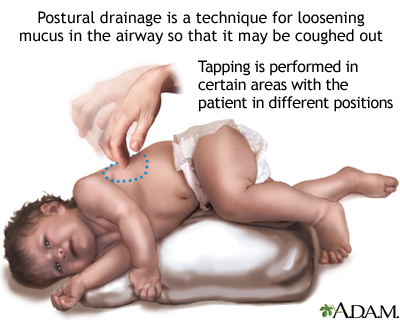
Lung problems are also treated with therapies to thin the mucus. This makes it easier to cough the mucus out of the lungs.
These methods include:
- Activity or exercise that causes you to breathe deeply
- Devices that are used during the day to help clear the airways of too much mucus
- Manual chest percussion (or chest physiotherapy), in which a family member or a therapist lightly claps the person's chest, back, and area under the arms
Treatment for bowel and nutritional problems may include:
- A special diet high in protein and calories for older children and adults
- Pancreatic enzymes to help absorb fats and protein, which are taken with every meal
- Vitamin supplements, especially vitamins A, D, E, and K
- Your provider can advise other treatments if you have very hard stools
Ivacaftor, lumacaftor, tezacaftor, and elexacaftor are medicines that treat certain types of CF.
- They improve the function of one of the defective genes that causes CF.
- Up to 90% of patients with CF and eligible for one or more of these medicines alone or in combination.
- As a result, there is less buildup of thick mucus in the lungs. Other CF symptoms are improved as well.
Care and monitoring at home should include:
- Avoiding smoke, dust, dirt, fumes, household chemicals, fireplace smoke, and mold or mildew.
- Giving plenty of fluids, especially to infants and children in hot weather, when there is diarrhea or loose stools, or during extra physical activity.
- Exercising 2 or 3 times each week. Swimming, jogging, and cycling are good options.
- Clearing or bringing up mucus or secretions from the airways. This must be done 1 to 4 times each day. Patients, families, and caregivers must learn about doing chest percussion and postural drainage to help keep the airways clear.
- No contact with other people with CF is recommended as they can exchange infections (does not apply to family members).
Support Groups
You can ease the stress of illness by joining a cystic fibrosis support group. Sharing with others who have common experiences and problems can help your family to not feel alone.
Outlook (Prognosis)
Most children with CF stay in good health until they reach adulthood. They are able to take part in most activities and attend school. Many young adults with CF finish college or find jobs.
Lung disease eventually worsens to the point where the person is disabled. Today, the average life span for people with CF who live to adulthood is about 44 years.
Death is most often caused by lung complications.
Possible Complications
The most common complication is chronic respiratory infection.
Other complications include:
- Bowel problems, such as gallstones, intestinal blockage, and rectal prolapse
- Coughing up blood
- Chronic respiratory failure
- Diabetes
- Infertility
- Liver disease or liver failure, pancreatitis, biliary cirrhosis
- Malnutrition
- Nasal polyps and sinusitis
- Osteoporosis and arthritis
- Pneumonia that keeps coming back
- Pneumothorax
- Right-sided heart failure (cor pulmonale)
- Colorectal cancer
When to Contact a Medical Professional
Call your provider if an infant or child has symptoms of CF, and experiences:
- Fever, increased coughing, changes in sputum or blood in sputum, loss of appetite, or other signs of pneumonia
- Increased weight loss
- More frequent bowel movements or stools that are foul-smelling or have more mucus
- Swollen belly or increased bloating
Call your provider if a person with CF develops new symptoms or if symptoms get worse, particularly severe breathing difficulty or coughing up blood.
Prevention
CF cannot be prevented. Screening those with a family history of the disease may detect the CF gene in many carriers.
Alternative Names
CF
References
Donaldson SH, Pilewski JM, Griese M, et al. Tezacaftor/ivacaftor in subjects with cystic fibrosis and F508del/F508del-CFTR or F508del/G551D-CFTR. Am J Respir Crit Care Med. 2018;197(2):214-224. PMID: 28930490 pubmed.ncbi.nlm.nih.gov/28930490/.
Eagan ME, Schechter MS, Voynow JA. Cystic fibrosis. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 432.
Farrell PM, White TB, Ren CL, et al. Diagnosis of cystic fibrosis: consensus guidelines from the Cystic Fibrosis Foundation. J Pediatr. 2017;181S:S4-S15.e1. PMID: 28129811 pubmed.ncbi.nlm.nih.gov/28129811/.
Graeber SY, Dopfer C, Naehrlich L, et al. Effects of lumacaftor/ivacaftor therapy on CFTR function in Phe508del homozygous patients with cystic fibrosis. Am J Respir Crit Care Med. 2018;197(11):1433-1442. PMID: 29327948 pubmed.ncbi.nlm.nih.gov/29327948/.
Grasemann H. Cystic fibrosis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 83.
Solomon GM, Hoover W, Sorscher EJ, Rowe SM. Cystic fibrosis: diagnosis and management. In: Broaddus VC, Ernst JD, King TE, Lazarus SC , Sarmiento KF, Schnapp LM, Stapleton RD, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 68.
Taylor-Cousar JL, Munck A, McKone EF, et al. Tezacaftor-ivacaftor in patients with cystic fibrosis homozygous for phe508del. N Engl J Med. 2017;377(21):2013-2023. PMID: 29099344 pubmed.ncbi.nlm.nih.gov/29099344/.
Review Date 2/24/2022
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






