Menopause is the time in a woman's life when her periods (menstruation) stop. Most often, it is a natural, normal body change that occurs between ages 45 to 55. After menopause, a woman can no longer become pregnant.
Causes
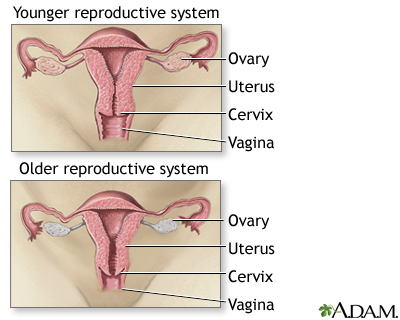
During menopause, a woman's ovaries stop releasing eggs. Her body produces less of the female hormones estrogen and progesterone. Lower levels of these hormones cause menopause symptoms.
Periods occur less often and eventually stop. Sometimes this happens suddenly. But most of the time, periods slowly stop over time.
Menopause is complete when you have not had a period for 1 year. This is called postmenopause. Surgical menopause takes place when surgical treatments cause a drop in estrogen. This can happen if both of your ovaries are removed.
Menopause can also sometimes be caused by drugs used for chemotherapy or hormone therapy (HT) for breast cancer.
Symptoms
Symptoms vary from woman to woman. They may last 5 or more years. Symptoms may be worse for some women than others. Symptoms of surgical menopause can be more severe and start more suddenly.
The first thing you may notice is that periods start to change. They might occur more often or less often. Some women might get their period every 3 weeks before starting to skip periods You may have irregular periods for 1 to 3 years before they stop completely.
Common symptoms of menopause include:
- Menstrual periods that occur less often and eventually stop
- Heart pounding or racing
- Hot flashes, usually worst during the first 1 to 2 years
- Night sweats
- Skin flushing
- Sleeping problems (insomnia)
Other symptoms of menopause may include:
- Decreased interest in sex or changes in sexual response
- Forgetfulness (in some women)
- Headaches
- Mood swings, including irritability, depression, and anxiety
- Urine leakage
- Vaginal dryness and painful sexual intercourse
- Vaginal infections
- Joint aches and pains
- Irregular heartbeat (palpitations)
Exams and Tests
Blood and urine tests can be used to look for changes in hormone levels. Test results can help your health care provider determine if you are close to menopause or if you have already gone through menopause. Your provider may need to repeat testing your hormone levels several times to confirm your menopausal status if you have not completely stopped menstruating.
Tests that may be done include:
Your provider will perform a pelvic exam. Decreased estrogen can cause changes in the lining of the vagina.
Bone loss increases during the first few years after your last period. Your provider may order a bone density test to look for bone loss related to osteoporosis. This bone density test is recommended for all women at age 65 if they have not already had it. This test may be recommended sooner if you are at higher risk for osteoporosis because of your family history or medicines that you take.
Treatment
Treatment may include lifestyle changes, HT, or both. Treatment depends on many factors such as:
- How bad your symptoms are
- Your overall health
- Your preferences
HORMONE THERAPY
HT may help if you have severe hot flashes, night sweats, mood issues, or vaginal dryness. HT is treatment with estrogen and, sometimes, progesterone.
Talk to your provider about the benefits and risks of HT. Your provider should be aware of your entire medical and family history before prescribing HT.
Several major studies have questioned the health benefits and risks of HT, including the risk of developing breast cancer, heart attacks, strokes, and blood clots. However, using HT for the 10 years after developing menopause is associated with a lower chance of death.
Current guidelines support the use of HT for the treatment of hot flashes. Specific recommendations are:
- HT may be started in women who have recently entered menopause.
- HT should not be used in women who started menopause many years ago, except for vaginal estrogen treatments.
- HT should not be used for longer than necessary. Some women may require prolonged estrogen use due to troublesome hot flashes. This is safe in healthy women.
- Women taking HT should have a low risk for stroke, heart disease, blood clots, or breast cancer.
To reduce the risks of estrogen therapy, your provider may recommend:
- A lower dose of estrogen or a different estrogen preparation (for instance, a vaginal cream or skin patch rather than a pill).
- Using patches appears to be safer than oral estrogen, as it avoids the increased risk for blood clots seen with oral estrogen use.
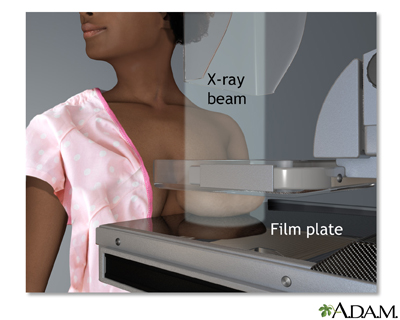
- Frequent and regular physical exams, including breast exams and mammograms
Women who still have a uterus (that is, have not had surgery to remove it for any reason) should take estrogen combined with progesterone to prevent cancer of the lining of the uterus (endometrial cancer).
ALTERNATIVES TO HORMONE THERAPY
There are other medicines that can help with mood swings, hot flashes, and other symptoms. These include:
- Antidepressants, including paroxetine (Paxil), venlafaxine (Effexor), bupropion (Wellbutrin), and fluoxetine (Prozac)
- A blood pressure medicine called clonidine
- Gabapentin, a seizure drug that also helps reduce hot flashes
DIET AND LIFESTYLE CHANGES
Lifestyle steps you can take to reduce menopause symptoms include:
Diet changes:
- Avoid caffeine, alcohol, and spicy foods.
- Eat soy containing foods. Soy contains estrogen.
- Get plenty of calcium and vitamin D in food or supplements.
Exercise and relaxation techniques:
- Get plenty of exercise.
- Do Kegel exercises every day. They strengthen the muscles of your vagina and pelvis.
- Practice slow, deep breathing whenever a hot flash begins. Try taking 6 breaths a minute.
- Try yoga, tai chi, or meditation.
Other tips:
- Dress lightly and in layers.
- Keep having sex.
- Use water-based lubricants or a vaginal moisturizer during sex if needed due to vaginal dryness.
- See an acupuncture specialist.
Possible Complications
Some women have vaginal bleeding after menopause. This is often nothing to worry about. However, you should tell your provider if this happens, especially if it occurs more than a year after menopause. It may be an early sign of problems such as cancer. Your provider may do a biopsy of the uterine lining, a vaginal ultrasound, or both.
Decreased estrogen level has been linked to some long-term effects, including:
- Bone loss and osteoporosis in some women
- Changes in cholesterol levels and greater risk for heart disease
When to Contact a Medical Professional
Contact your provider if:
- You are spotting blood between periods
- You have had 12 consecutive months with no period and vaginal bleeding or spotting begins again suddenly (even a small amount of bleeding)
Prevention
Menopause is a natural part of a woman's life. It does not need to be prevented. You can reduce your risk for long-term problems such as osteoporosis and heart disease by taking the following steps:
- Control your blood pressure, cholesterol, and other risk factors for heart disease.
- Do not smoke. Cigarette use can cause early menopause.
- Get regular exercise. Resistance exercises help strengthen your bones and improve your balance.
- Talk to your provider about medicines that can help stop further bone weakening if you show early signs of bone loss or have a strong family history of osteoporosis.
- Take calcium and vitamin D.
Alternative Names
Perimenopause; Postmenopause
Images
References
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123(1):202-216. PMID: 24463691 pubmed.ncbi.nlm.nih.gov/24463691/.
Lobo RA. Menopause and care of the mature woman: endocrinology, consequences of estrogen deficiency, effects of hormone therapy, and other treatment options. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 14.
North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. PMID: 35797481 pubmed.ncbi.nlm.nih.gov/28650869/.
Rushing J, Skaznik-Wikiel ME, Santoro N. Menopause and perimenopause. In: Robertson RP ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 122.
US Preventive Services Task Force, Grossman DC, Curry SJ, et al, eds. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(15):1592-1599. PMID: 29677309 pubmed.ncbi.nlm.nih.gov/29677309/.
Van den Beld AW, Lamberts SWJ. Endocrinology and aging. In: Melmed S, Auchus, RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 28.
Test Your Knowledge
Review Date 7/12/2023
Updated by: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.





