Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel disease (IBD). Crohn disease is another form of IBD.
Causes
The cause of ulcerative colitis is unknown. People with this condition have problems with their immune system. However, it is not clear if immune problems cause this illness. Stress and certain foods can trigger symptoms, but they do not cause ulcerative colitis.
Ulcerative colitis may affect any age group. The peaks in the age of onset occurs at ages 15 to 30 and then again at ages 50 to 70.
The disease begins in the rectal area. It may stay in the rectum or spread to higher areas of the large intestine. However, the disease does not skip areas. It may involve the entire large intestine over time.
Risk factors include a family history of ulcerative colitis or other autoimmune diseases, or Jewish ancestry.
Symptoms
The symptoms can be more or less severe. They may start slowly or suddenly. Half of people only have mild symptoms. Others have more severe attacks that occur more often. Many factors can lead to attacks.
Symptoms may include:
- Pain in the abdomen (belly area) and cramping.
- A gurgling or splashing sound heard over the intestine.
- Blood and possibly pus in the stools.
- Diarrhea, from only a few episodes to very often.
- Fever.
- Feeling that you need to pass stools, even though your bowels are already empty (tenesmus). It may involve straining, pain, and cramping.
- Weight loss.
Children's growth may slow.
Other symptoms that may occur with ulcerative colitis include the following:
- Eye irritation
- Joint pain and swelling
- Nausea and vomiting
- Skin lumps or ulcers
Exams and Tests
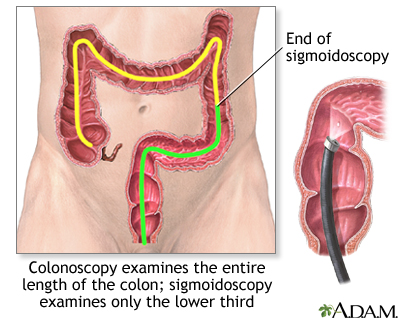
Colonoscopy with biopsy is most often used to diagnose ulcerative colitis. Colonoscopy is also used to screen people with ulcerative colitis for colon cancer.
Other tests that may be done to help diagnose this condition include:
- Barium enema
- Complete blood count (CBC)
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Stool calprotectin or lactoferrin
- Antibody tests of the blood
Sometimes, tests of the small intestine are needed to differentiate between ulcerative colitis and Crohn disease, including:
- CT scan
- MRI
- Upper endoscopy or capsule endoscopy
- MR enterography
Treatment
The goals of treatment are to:
- Control the acute attacks
- Prevent repeated attacks
- Help the colon heal
During a severe episode, you may need to be treated in the hospital. Your health care provider may prescribe corticosteroids. You may be given nutrients through a vein (IV line).
DIET AND NUTRITION
Certain types of foods may worsen diarrhea and gas symptoms. This problem may be more severe during times of active disease. Diet suggestions include:
- Eat small amounts of food throughout the day.
- Drink plenty of water (drink small amounts throughout the day).
- Avoid high-fiber foods (bran, beans, nuts, seeds, and popcorn).
- Avoid fatty, greasy or fried foods and sauces (butter, margarine, and heavy cream).
- Limit milk products if you are lactose intolerant. Dairy products are a good source of protein and calcium.
STRESS
You may feel worried, embarrassed, or even sad or depressed about having a bowel accident. Other stressful events in your life, such as moving, or losing a job or a loved one can cause worsening of digestive problems.
Ask your provider for tips about how to manage your stress.
MEDICINES
You can take medicine to treat very bad diarrhea. Loperamide (Imodium) can be bought without a prescription. Always talk to your provider before using these drugs.
Medicines that may be used to decrease the number of attacks include:
- 5-aminosalicylates such as mesalamine or sulfasalazine, which can help control moderate symptoms. Some forms of the drug are taken by mouth. Others must be inserted into the rectum.
- Medicines to quiet the immune system.
- Corticosteroids such as prednisone. They may be taken by mouth during a flare-up or inserted into the rectum.
- Immunomodulators, medicines taken by mouth that affect the immune system, such as azathioprine and 6-MP.
- Biologic therapy, if you do not respond to other drugs.
- Acetaminophen (Tylenol) may help relieve mild pain. Avoid drugs such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn). These can make your symptoms worse.
SURGERY
Surgery to remove the colon will cure ulcerative colitis and removes the threat of colon cancer. You may need surgery if you have:
- Colitis that does not respond to intensive medical therapy
- Changes in the lining of the colon that suggests an increased risk for cancer
- Severe problems, such as rupture of the colon, severe bleeding, or toxic megacolon
Most of the time, the entire colon, including the rectum, is removed. After surgery, you may have:
- An opening in your belly called the stoma (ileostomy). Stool will drain out through this opening.
- A procedure that connects the small intestine to the anus to gain more normal bowel function.
Support Groups
Social support can often help with the stress of dealing with illness, and support group members may also have useful tips for finding the best treatment and coping with the condition.
More information and support for people with Crohn disease and their families can be found at:
Outlook (Prognosis)
Symptoms are mild in about one half of people with ulcerative colitis. More severe symptoms are less likely to respond well to medicines.
Cure is only possible through complete removal of the large intestine.
The risk for colon cancer increases in each decade after ulcerative colitis is diagnosed.
Possible Complications
You have a higher risk for small bowel and colon cancer if you have ulcerative colitis. At some point, your provider will recommend tests to screen for colon cancer.
More severe episodes that recur may cause the walls of the intestines to become thickened, leading to:
- Colon narrowing or blockage (more common in Crohn disease)
- Episodes of severe bleeding
- Severe infections
- Sudden widening (dilation) of the large intestine within one to a few days (toxic megacolon)
- Tears or holes (perforation) in the colon
- Anemia, low blood count
Problems absorbing nutrients may lead to:
- Problems maintaining a healthy weight
- Slow growth and development in children
- Anemia or low blood count
Less common problems that may occur include:
- A type of arthritis that affects the bones and joints at the base of the spine, where it connects with the pelvis (ankylosing spondylitis)
- Liver disease
- Tender, red bumps (nodules) under the skin, which may turn into skin ulcers
- Inflammation in the eye
When to Contact a Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
Prevention
There is no known prevention for this condition.
Alternative Names
Inflammatory bowel disease - ulcerative colitis; IBD - ulcerative colitis; Colitis; Proctitis; Ulcerative proctitis
Patient Instructions
- Bland diet
- Changing your ostomy pouch
- Diarrhea - what to ask your health care provider - adult
- Ileostomy and your child
- Ileostomy and your diet
- Ileostomy - caring for your stoma
- Ileostomy - changing your pouch
- Ileostomy - discharge
- Ileostomy - what to ask your doctor
- Large bowel resection - discharge
- Living with your ileostomy
- Low-fiber diet
- Total colectomy or proctocolectomy - discharge
- Types of ileostomy
- Ulcerative colitis - discharge
References
Ananthakrishnan AN, Reguerio MD. Management of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Cameron J. Large bowel. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:177-286.
Galandiuk S, Netz U, Morpurgo E, Tosato SM, Abu-Freha N, Ellis CT. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 52.
Kaplan GG, Ng SC. Epidemiology, pathogenesis, and diagnosis of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 115.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 127.
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guidelines: ulcerative colitis in adults. Am J Gastroenterol. 2019:114(3):384-413. PMID: 30840605 pubmed.ncbi.nlm.nih.gov/30840605/.
Review Date 2/6/2022
Updated by: Internal review and update on 07/16/2023 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Internal review and update on 02/10/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.





