Uterine fibroids are tumors that grow in a woman's womb (uterus). These growths are typically not cancerous (benign), and do not become cancerous.
Causes
Uterine fibroids are common. As many as one in five women may have fibroids during their childbearing years. Half of all women have fibroids by age 50.
Fibroids are rare in women under age 20. They are more common in African Americans than White, Hispanic, or Asian women.
No one knows exactly what causes fibroids. They are thought to be caused by:
- Hormones in the body
- Genes (may run in families)
Fibroids can be so tiny that you need a microscope to see them. They can also grow very large. They may fill the entire uterus and may weigh several pounds or kilograms. Although it is possible for just one fibroid to develop, most often there is more than one.
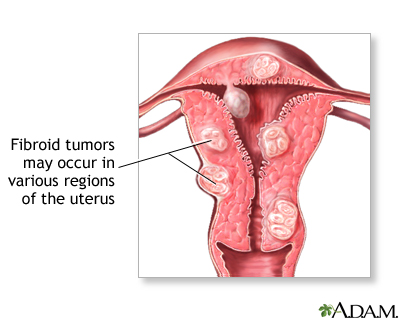
Fibroids can grow:
- In the muscle wall of the uterus (myometrial)
- Just under the surface of the uterine lining (submucosal)
- Just under the outside lining of the uterus (subserosal)
- On a long stalk on the outside the uterus or inside the uterus (pedunculated)
Symptoms
Common symptoms of uterine fibroids are:
- Bleeding between periods
- Heavy bleeding during your period, sometimes with blood clots
- Periods that may last longer than normal
- Needing to urinate more often
- Pelvic cramping or pain with periods
- Feeling fullness or pressure in your lower belly
- Pain during intercourse
Often, you can have fibroids and not have any symptoms. Your health care provider may find them during a physical exam or other test. Fibroids often shrink and cause no symptoms in women who have gone through menopause. A recent study also showed that some small fibroids shrink in premenopausal women.
Exams and Tests
Your provider will perform a pelvic exam. This may show that you have a change in the shape and size of your womb.
Fibroids are not always easy to diagnose. Being obese may make fibroids harder to detect. You may need these tests to look for fibroids:
- Ultrasound uses sound waves to create a picture of the uterus.
- MRI uses powerful magnets and radio waves to create a picture.
- Saline infusion sonogram (hysterosonography) -- Saline is injected into the uterus to make it easier to see the uterus using ultrasound.
- Hysteroscopy uses a long, thin tube inserted through the vagina and into the uterus to examine the inside of the uterus.
- Endometrial biopsy removes a small piece of the lining of the uterus to check for cancer if you have unusual bleeding.
Treatment
What type of treatment you have depends on:
- Your age
- Your general health
- Your symptoms
- Type of fibroids
- If you are pregnant
- If you want children in the future
Treatment for the symptoms of fibroids may include:
- Intrauterine devices (IUDs) that release hormones to help reduce heavy bleeding and pain.
- Tranexamic acid to reduce the amount of blood flow.
- Iron supplements to prevent or treat anemia due to heavy periods.
- Pain relievers, such as ibuprofen or naproxen, for cramps or pain.
- Watchful waiting -- You may have follow-up pelvic exams or ultrasounds to check the fibroid's growth.
Medical or hormonal therapies that may help shrink fibroids include:
- Birth control pills to help control heavy periods.
- A type of IUD that releases a low dose of the hormone progestin into the uterus each day.
- Hormone shots to help shrink fibroids by stopping ovulation. Most often, this therapy is used only for a short time to shrink fibroids before surgery. They can also be used longer when small amounts of estrogen hormone are added back to reduce side effects.
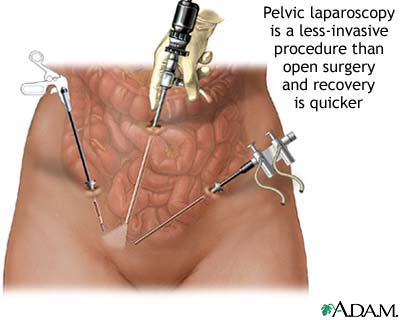
Surgery and procedures used to treat fibroids include:
- Hysteroscopy -- This procedure can remove fibroids growing inside the uterus.
- Endometrial ablation -- This procedure is sometimes used to treat heavy bleeding associated with fibroids. It works best when the fibroids are small in size. It often stops menstruation completely.
- Uterine artery embolization -- This procedure stops the blood supply to the fibroid, causing it to shrink and die. This may be a good option if you wish to avoid surgery and are not planning to become pregnant.
- Myomectomy -- This surgery removes the fibroids from the uterus. This also may be a good choice if you want to have children. It will not prevent new fibroids from growing.
- Hysterectomy -- This surgery removes the uterus completely. It may be an option if you do not want children, medicines do not work, and you cannot have any other procedures.
Newer treatments, such as the use of focused ultrasound, are being evaluated in clinical studies.
Outlook (Prognosis)
If you have fibroids without symptoms, you may not need treatment.
If you have fibroids, they may grow if you become pregnant. This is due to the increased blood flow and higher estrogen levels. The fibroids usually return to their original size after your baby is born.
Possible Complications
Complications of fibroids include:
- Severe pain or very heavy bleeding that needs emergency surgery.
- Twisting of the fibroid -- This can cause blocked blood vessels that feed the tumor. You may need surgery if this happens.
- Anemia (not having enough red blood cells) from heavy bleeding.
- Urinary tract infections -- If the fibroid presses on the bladder, it can be hard to empty your bladder completely.
- Infertility, in rare cases.
If you are pregnant, there's a small risk that fibroids may cause complications:
- You may deliver your baby early because there is not enough room in your womb.
- If the fibroid blocks the birth canal or puts the baby in a dangerous position, you may need to have a cesarean section (C-section).
- You may have heavy bleeding right after giving birth.
When to Contact a Medical Professional
Contact your provider if you have:
- Heavy bleeding, increased cramping, or bleeding between periods
- Fullness or heaviness in your lower belly area
Alternative Names
Leiomyoma; Fibromyoma; Myoma; Fibroids; Uterine bleeding - fibroids; Vaginal bleeding - fibroids
References
Bulun SE. Physiology and pathology of the female reproductive axis. In: Melmed S, Auchus, RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 17.
Dolan MS, Hill CC, Valea FA. Benign gynecologic lesions: vulva, vagina, cervix, uterus, oviduct, ovary, ultrasound imaging of pelvic structures. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 18.
Manyonda I, Belli AM, Lumsden MA, et al. Uterine-artery embolization or myomectomy for uterine fibroids. N Engl J Med. 2020 ;383(5):440-451. PMID: 32726530 pubmed.ncbi.nlm.nih.gov/32726530/.
Moravek MB, Bulun SE, Stewart EA, Orellana M. Uterine fibroids and adenomyosis. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier;2023:chap 126.
Verpalen IM, Anneveldt KJ, Nijholt IM, et al. Magnetic resonance-high intensity focused ultrasound (MR-HIFU) therapy of symptomatic uterine fibroids with unrestrictive treatment protocols: a systematic review and meta-analysis. Eur J Radiol. 2019;120:108700. doi: 10.1016/j.ejrad.2019.108700. PMID: 31634683 pubmed.ncbi.nlm.nih.gov/31634683/.
Review Date 1/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Internal review and update on 07/25/2023 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






