COMMUNITY HEALTH
|
A SIMPLE SOLUTION
"Small is beautiful but big is necessary."—BRAC motto, 1970s
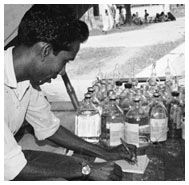
Teaching oral rehydration therapy, Bangladesh, 1980s
Courtesy BRAC Bangladesh
Oral rehydration therapy (ORT) is an inexpensive, life-saving treatment for dehydration. Wherever access to clean water and sanitation is limited, diarrheal diseases
like cholera threaten lives, especially those of babies and young children. ORT, which is essentially a mixture of salt, water, and sugar, has earned the label "a simple
solution" because it is made from basic, inexpensive ingredients, and can be easily learned.
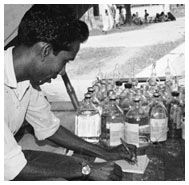
 Clinic staff at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967
Clinic staff at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967Courtesy Mrs. Elizabeth B. Gordon
Scientists around the world have contributed to the development of ORT. Over the last two hundred years, researchers have experimented with the
ingredients of centuries-old traditional treatments, to refine and perfect a therapy to replenish lost nutrients. In the second half of the twentieth
century these efforts intensified. Between 1966 and 1968, two groups, the Pakistan-SEATO Cholera Research Laboratory, (PSCRL) and the Johns Hopkins Center
for Medical Research and Training, (JH-CMRT) established the benefits of the solution.
 Dr. ASM Mizanur Rahman, chief clinician at Matlab, East Pakistan, 1968
Dr. ASM Mizanur Rahman, chief clinician at Matlab, East Pakistan, 1968Courtesy David R. Nalin, M.D.
In 1968, Dr. ASM Mizanur Rahaman led a study to test ORT at Matlab, a treatment center without electricity and limited medical supplies. Colleagues Richard Cash and David Nalin treated 150 cholera patients and proved that the technique could help people recover even when few other resources were available.
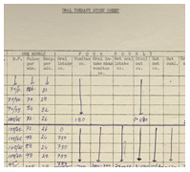 Bedside datasheet from the first successful demonstration of ORT, Dacca, East Pakistan, 1968
Bedside datasheet from the first successful demonstration of ORT, Dacca, East Pakistan, 1968Courtesy David R. Nalin, M.D.
In April 1968, researcher David Nalin successfully treated patients at the PSCRL using a glucose-sodium oral solution. Nurses treated three groups of patients and found that the amount of fluid needed to rehydrate patients was reduced by 80 percent. This proved that ORT helped the body absorb fluids more efficiently. The next step was to determine whether it could be used outside a hospital setting.
 Ambulance speedboat used to bring patients to the Matlab treatment center, East Pakistan, 1970s
Ambulance speedboat used to bring patients to the Matlab treatment center, East Pakistan, 1970sCourtesy David R. Nalin, M.D.
 The main ward of the hospital at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967
The main ward of the hospital at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967Courtesy David R. Nalin, M.D.
Because of a long history of endemic cholera, East Pakistan (now Bangladesh) was chosen by researchers as the location to conduct long-term studies on oral rehydration therapy (ORT). In October 1960 the American and Pakistani governments signed a formal agreement to establish the Pakistan-SEATO Cholera Research Laboratory for this work in Dacca (now Dhaka). The first successful clinical trials of ORT were carried out here.
 Matlab treatment center, East Pakistan, 1964
Matlab treatment center, East Pakistan, 1964Courtesy Mrs. Elizabeth B. Gordon
PSCRL's hospital was supplemented by a diarrheal treatment facility at the Matlab Center, originally housed on a barge that had previously served as a prison in East Pakistan (later Bangladesh). This facility was started in 1966, supported by speedboat and jeep ambulances that transported patients from villages in the Meghna river basin.
 PSCRL jeep ambulance, East Pakistan, 1965
PSCRL jeep ambulance, East Pakistan, 1965Courtesy Mrs. Elizabeth B. Gordon
 Administering oral rehydration therapy, Bangladesh, 1980s
Administering oral rehydration therapy, Bangladesh, 1980sCourtesy ICDDR,B
The Johns Hopkins Center for Medical Research and Training refugee camp
The Matlab field trial proved to the medical community that ORT could be employed in rural settings, but it was still unknown whether it would be effective in large-scale emergencies. Around the same time as the PSCRL breakthroughs, the Johns Hopkins Center for Medical Research and Training (JH-CMRT) was also working on cholera treatment in Calcutta, India. In the summer of 1968, Nalin went to Calcutta to share his findings with the JH-CMRT.
 Cholera refugees, East Pakistan, 1971
Cholera refugees, East Pakistan, 1971Courtesy Thomas Simpson, M.D.
In May 1971, the Liberation War between East and West Pakistan (which led to the creation of Bangladesh), displaced approximately ten million people. They were housed in refugee camps in West Bengal, India. When monsoon season arrived in June, a cholera epidemic spread throughout the camps. Tired, malnourished, and living in unsanitary conditions, many refugees became seriously ill. Before aid arrived at the camp almost one
third of the inhabitants died from cholera and diarrheal disease.
 2002 Pollin Prize in Pediatric Research winners (left to right) Nathaniel Pierce, David Nalin, Norbert Hirschorn, Rudi Leiber, Dilip Mahalanabis
2002 Pollin Prize in Pediatric Research winners (left to right) Nathaniel Pierce, David Nalin, Norbert Hirschorn, Rudi Leiber, Dilip MahalanabisCourtesy David R. Nalin, M.D.
Mahalanabis and his colleagues proved that ORT could be administered by people who had no previous health care training, and that the therapy was effective in large-scale emergencies. In recognition of the importance of this work, the group received the first Pollin Prize in Pediatric Research, in 2002.
 Depleted supply of intravenous fluid, 1971
Depleted supply of intravenous fluid, 1971Courtesy Thomas Simpson, M.D.
Given the large numbers of people with cholera in refugee camps it was impossible to supply enough intravenous fluid to treat dehydration. JH-CMRT decided that administering ORT would be the most practical treatment solution, and on June 24, 1971 Dr. Dilip Mahalanabis set up two ORT teams in Bongaon, India, near the East Pakistan-India border. From June 24 to August 30 they treated approximately four thousand people with
cholera with ORT. Towards the end of June, the peak of the epidemic, more than two hundred new patients were admitted for treatment each day. The overwhelmed staff could not keep up, and family members had to help by feeding ORT to ailing relatives and friends.
Bangladesh Rural Advancement Committee (BRAC)
 F. H. Abed, founder of the Bangladesh Rural Advancement Committee (BRAC), 1990s
F. H. Abed, founder of the Bangladesh Rural Advancement Committee (BRAC), 1990sCourtesy BRAC Bangladesh
Fazle Hasan Abed, a former accountant, founded the Bangladesh Rural Advancement Committee (BRAC) in 1972 to help in the recovery of the country after the Liberation War of 1971. What began as a small, private organization has since expanded across the country and into Afghanistan.
 A BRAC worker gives a lesson, 1980s
A BRAC worker gives a lesson, 1980sCourtesy BRAC Bangladesh
BRAC was able to reach a large proportion of the population by training local women to visit communities across the country. "Small is beautiful but big is necessary" is the organization's motto, illustrating their vision of teaching every family in the country this life-saving technique.
 BRAC bag containing teaching materials, mixing cup and spoon, ca. 2006
BRAC bag containing teaching materials, mixing cup and spoon, ca. 2006Courtesy BRAC Bangladesh
 BRAC team traveling to mountain communities, Afghanistan, 2006
BRAC team traveling to mountain communities, Afghanistan, 2006Courtesy BRAC Bangladesh
BRAC has recently expanded into Afghanistan, which faces many of the same problems that were present in Bangladesh when the organization was founded. Health in the region has been undermined by conflict, and medical staff and facilities are desperately needed. BRAC has been able to deliver health services to isolated
rural communities by traveling into mountainous regions of the country.
 A BRAC teacher measures a pinch of salt, 1980s
A BRAC teacher measures a pinch of salt, 1980sCourtesy BRAC Bangladesh
 A villager learning how to make ORT measures out water, 1980s
A villager learning how to make ORT measures out water, 1980sCourtesy BRAC Bangladesh
The easy-to-learn formula for oral rehydration therapy, made by mixing salt and sugar with water, is taught as "one pinch and one fist." Fazle Hasan Abed perfected the measurements through trial and error in his kitchen.
 BRAC workers traveling to communities, 1980s
BRAC workers traveling to communities, 1980sCourtesy BRAC Bangladesh
Women between the ages of twenty and fifty are recruited by BRAC to teach oral rehydration therapy. Because Bangladeshi culture does not always allow women to travel far from their homes, men chaperone the workers and introduce them at each village they visit.
 BRAC community health worker teaching oral rehydration therapy, Balkh Province, Afghanistan, 2006
BRAC community health worker teaching oral rehydration therapy, Balkh Province, Afghanistan, 2006Courtesy BRAC Bangladesh
Oral rehydration therapy in Egypt
Diarrhea was the number one killer of children in Egypt in the late 1970s, thought to be responsible for half of all the nation's infant deaths. From 1981 to 1991 the Egyptian government carried out a major campaign to promote oral rehydration therapy, reducing the country's child mortality rate by one third.
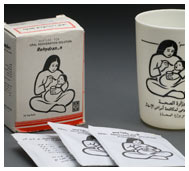 Packets of oral rehydration solution and cup featuring the campaign icon of a mother and child, 1980s
Packets of oral rehydration solution and cup featuring the campaign icon of a mother and child, 1980sCourtesy Norbert Hirschhorn, M.D.
Rather than using the homemade version of the solution, the program relied upon the sale of commercially-produced packets, subsidized by the government and funding from the United States Agency for International Development (USAID). Many Egyptian parents could no longer afford the treatment when the subsidies ended.
 Calendar showing how to make oral rehydration solution, 1989
Calendar showing how to make oral rehydration solution, 1989Courtesy Farag Elkamel, Ph.D
 Promoting the use of oral rehydration therapy, Egypt, 1980s
Promoting the use of oral rehydration therapy, Egypt, 1980sCourtesy Farag Elkamel, Ph.D.
Next

 Clinic staff at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967
Clinic staff at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967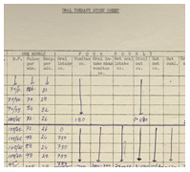 Bedside datasheet from the first successful demonstration of ORT, Dacca, East Pakistan, 1968
Bedside datasheet from the first successful demonstration of ORT, Dacca, East Pakistan, 1968 The main ward of the hospital at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967
The main ward of the hospital at the Pakistan-SEATO Cholera Research Laboratory, Dacca, 1967 2002 Pollin Prize in Pediatric Research winners (left to right) Nathaniel Pierce, David Nalin, Norbert Hirschorn, Rudi Leiber, Dilip Mahalanabis
2002 Pollin Prize in Pediatric Research winners (left to right) Nathaniel Pierce, David Nalin, Norbert Hirschorn, Rudi Leiber, Dilip Mahalanabis F. H. Abed, founder of the Bangladesh Rural Advancement Committee (BRAC), 1990s
F. H. Abed, founder of the Bangladesh Rural Advancement Committee (BRAC), 1990s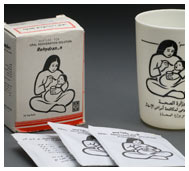 Packets of oral rehydration solution and cup featuring the campaign icon of a mother and child, 1980s
Packets of oral rehydration solution and cup featuring the campaign icon of a mother and child, 1980s